Diabetes is a complex, chronic condition characterized by high levels of glucose (sugar) in the blood. This occurs either because the body does not produce enough insulin, or because the cells stop responding to the insulin that is produced. With the prevalence of diabetes rising globally, understanding its distinct causes is the first step toward prevention and management.
While the symptoms—fatigue, increased thirst and urination—may overlap, the two primary types of diabetes, Type 1 and Type 2, have fundamentally different origins, risk factors, and mechanisms of development.
🛑 Type 1 Diabetes: The Immune System Attack
Type 1 diabetes (T1D), historically known as juvenile diabetes, is an autoimmune disease. In T1D, the root cause is the body’s immune system mistakenly identifying its own insulin-producing cells as foreign invaders.
The Autoimmune Mechanism
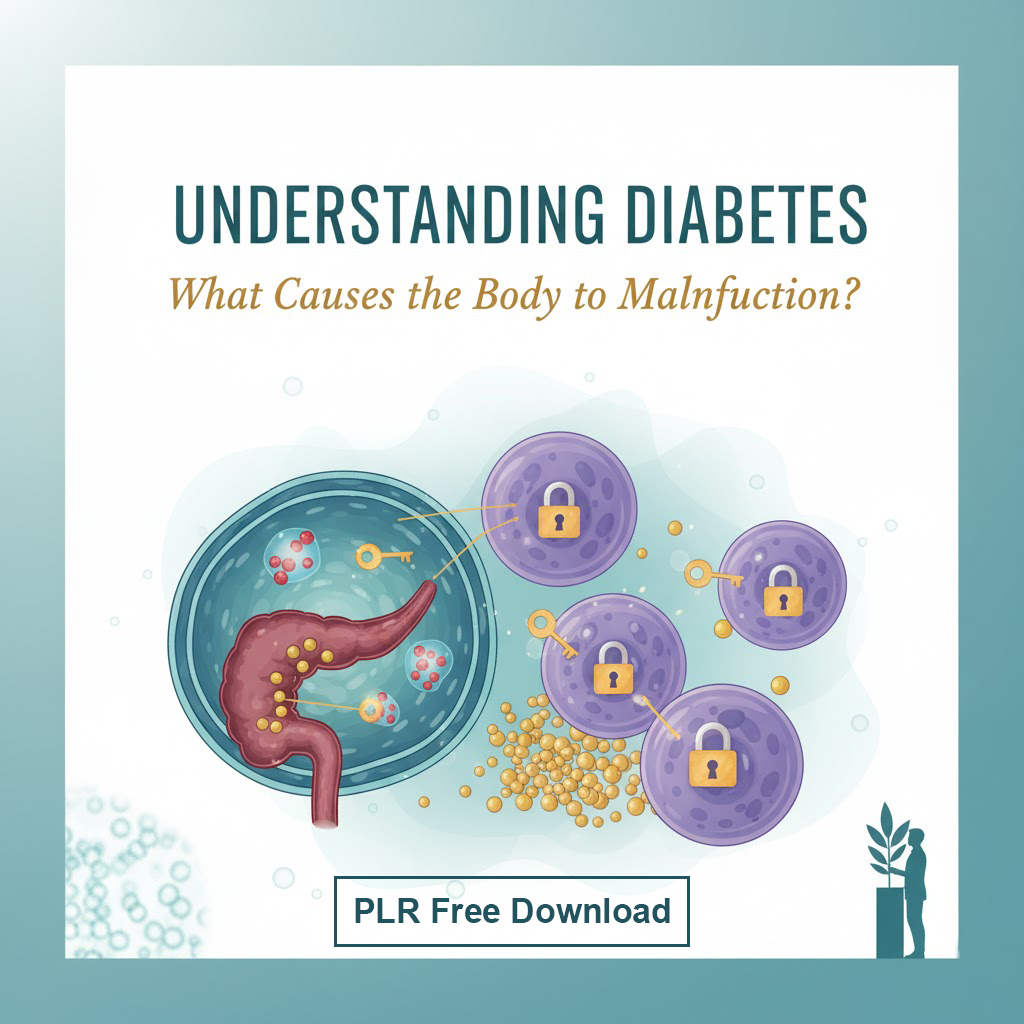
The body’s immune cells, specifically T-cells, launch an attack on the beta cells located in the islets of Langerhans within the pancreas. These beta cells are responsible for producing and releasing insulin. The attack slowly but surely destroys these cells, eventually leading to an absolute deficiency of insulin.
- Insulin Deficiency: Without insulin, glucose cannot enter the body’s cells for energy and instead accumulates in the bloodstream, leading to hyperglycemia (high blood sugar).
- Rapid Onset: Symptoms tend to develop quickly, often over days or weeks, particularly in children and adolescents. Though it can be diagnosed at any age, it is more common in younger individuals.
Key Causal Factors of Type 1 Diabetes
The exact trigger for this autoimmune response is not fully understood, but it is believed to be a combination of genetic predisposition and environmental factors:
- Genetic Susceptibility: T1D has a clear genetic component. Individuals with certain human leukocyte antigen (HLA) genes are at a significantly higher risk. If a close family member (parent or sibling) has T1D, the risk increases.
- Environmental Triggers: Researchers believe that in genetically susceptible individuals, an environmental trigger—such as a viral infection (like coxsackievirus)—may initiate the autoimmune attack. The virus may mimic a beta cell protein, causing the immune system to attack both the virus and the healthy pancreatic cells.
- Pancreatic Damage: Less commonly, Type 1 diabetes can be the result of severe damage to the pancreas due to external factors, such as injury, surgery, or chronic pancreatitis, which destroys insulin-producing tissue.
T1D requires lifelong treatment with external insulin to replace what the body can no longer produce.
📈 Type 2 Diabetes: Lifestyle, Resistance, and Exhaustion
Type 2 diabetes (T2D) accounts for about 90–95% of all diabetes cases and has a different, far more complex set of causes. The core issue in T2D is not a lack of insulin, but the body’s impaired response to it.
The Core Problem: Insulin Resistance
Initially, the pancreas produces insulin, but the muscle, fat, and liver cells in the body do not use it effectively. This is known as insulin resistance.
- Glucose Blockage: Insulin acts like a key to unlock cell doors, allowing glucose to enter and be used for energy. With resistance, the lock is jammed, and glucose remains in the blood.
- Pancreatic Overdrive: To overcome this resistance, the pancreas works overtime, producing increasing amounts of insulin to try and lower blood sugar. Over many years, this unsustainable demand can lead to beta cell exhaustion and failure. The pancreas eventually loses its ability to produce enough insulin to maintain normal glucose levels.
The Primary Risk Factors and Triggers
While genetics play a role, T2D is fundamentally a disease driven by modern lifestyle factors.
1. Chronic Weight and Sedentary Lifestyle
This is the most significant preventable cause.
- Obesity and Visceral Fat: Carrying excess body weight, particularly visceral fat (fat stored around the abdominal organs), is strongly linked to insulin resistance. Fat cells, especially those in the abdomen, release chemicals that interfere with the action of insulin in muscle and liver cells.
- Inactivity: A sedentary lifestyle reduces the body’s muscle mass and decreases its ability to utilize glucose, exacerbating resistance. Physical activity, conversely, makes cells more sensitive to insulin.
2. Diet and Chronic Over-nutrition
A diet characterized by constant high-calorie intake, especially from refined carbohydrates and sugars, drives the cycle of insulin resistance.
- Constant Glucose Load: Consuming a diet rich in refined sugars and starches leads to a constant influx of glucose into the bloodstream, requiring the pancreas to continually produce high levels of insulin. This sustained overproduction is what ultimately leads to the exhaustion of the beta cells.
3. Genetics and Family History
T2D has a stronger hereditary link than T1D. A person’s risk increases if a parent or sibling has the disease, suggesting that genetic predisposition makes some individuals more susceptible to developing insulin resistance when confronted with poor lifestyle factors.
4. The “Chicken-and-Egg” of Other Conditions
Other health issues commonly coexist with and may accelerate the development of T2D:
- High Blood Pressure (Hypertension): Hypertension is frequently observed alongside insulin resistance. While the exact causal link is complex, research suggests that high blood pressure may damage blood vessel linings, impairing the efficiency of glucose delivery and worsening resistance.
- Chronic Stress: Prolonged, unmanaged stress triggers the release of stress hormones, primarily cortisol. Cortisol’s function is to raise blood sugar to provide immediate energy for a threat. Chronic elevation of these hormones forces the pancreas into constant overdrive and exacerbates insulin resistance, significantly increasing diabetes risk.
- Abnormal Cholesterol Levels (Dyslipidemia): Low levels of “good” HDL cholesterol and high levels of triglycerides are part of a cluster of risk factors, often referred to as Metabolic Syndrome, that highly predict the onset of Type 2 diabetes.
Understanding these two different pathways—the autoimmune attack of T1D versus the lifestyle-driven insulin resistance of T2D—is vital for recognizing symptoms and implementing the necessary treatments or, for Type 2, the powerful preventative measures available.